By now you have probably seen firsthand or at least heard about the benefits of using capnography in an anesthetized patient. This monitor provides us with critical information about the ventilatory status, status of metabolism, pulmonary perfusion and therefore cardiac output in our anesthetized patients. We can gain valuable information about our patients from both the numerical values and the waveform displayed. But did you know that it also provides us with vital information about the integrity and function of our equipment? Yes! That’s correct! The capnograph can also give us valuable information about our anesthesia circuits, anesthetic machines, ET tubes dead space and flowrates. This article will outline what you will see on your capnograph when your equipment needs a little TLC.
As an RVT who travels to different clinics providing anesthesia the Capnograph is my most important monitor for catching issues with the anesthetic equipment before they become a problem. First, let’s review what a normal capnograph waveform looks like.
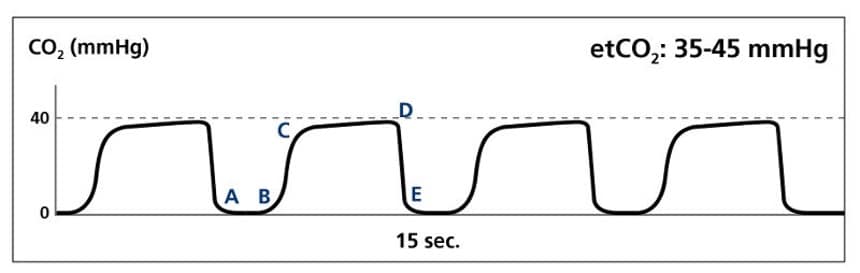
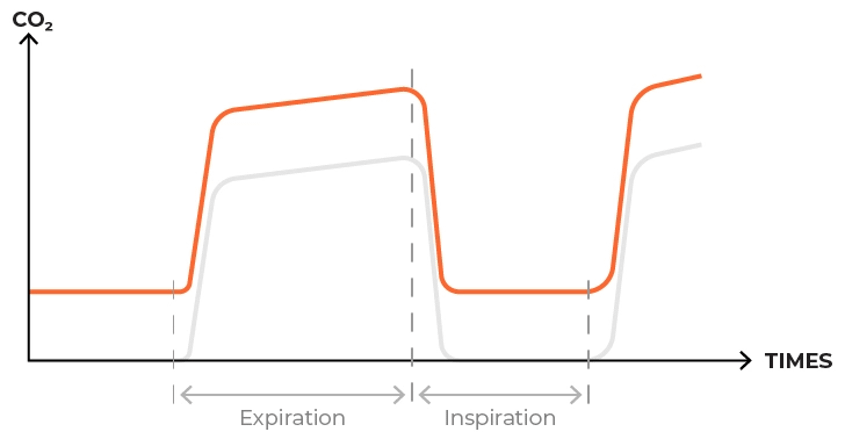
Image from https://www.ems1.com/capnography/infographic-understanding-normal-and-abnormal-capnography-waveforms
- A-B: Baseline this value should be 0
- B-C: Expiratory Upstroke, a continued exhalation of a mixture of dead space gas (from airway) and alveolar gas (from lungs)
- C-D: Alveolar Plateau, continued exhalation of alveolar gas
- D: Peak of plateau represents End Tidal CO2 (EtCO2)
- D-E: Inspiratory Downstroke, inhalation, rapid decrease in EtCO2, reaches 0
- Normal EtCO2 values are between 35-45mmHg.
There are lots of scenarios when your capnograph waveform and values would stray from the normal. This article will focus on increased InCO2/FiCO2 values or when your capnograph waveform does not return to zero in between exhalations. This can cause your EtCO2 values to get dangerously high!
So, what is InCO2 or FiCO2?
Incoming CO2 (InCO2) or Fraction of inspired CO2 (FiCO2), depending on the monitor you have you will see one or the other displayed, is the amount of CO2 left in the anesthetic breathing circuit at the beginning of inspiration. This is known as rebreathing. This value should be zero, as our patient should not be inspiring CO2, and depicted on the capnograph by returning to the baseline in between exhalations. If you are getting values other than zero, after checking your patient, you should focus your troubleshooting efforts on your anesthetic equipment. If left untreated, rebreathing CO2 can lead to hypoxic gas mixtures (Lumb).
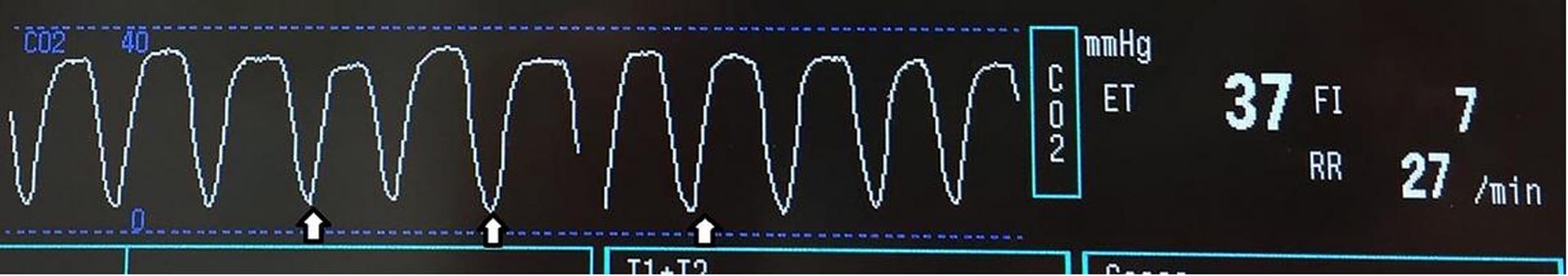
Image from www.bvna.org.uk
My capnograph waveform is not returning to a baseline of zero and my InCO2/FiCO2 value isn’t zero!! What should I do?
Troubleshooting Checklist:
- Ensure your ET tube is the appropriate length. Remember a long ET tube increases mechanical dead space which allows for the mixing of inspired and expired gases. The length of the ET tube should reach from the tip of the patient’s incisors to the thoracic inlet (GRUBB). To decrease dead space, it may be necessary to cut the ET tube to the appropriate length. Just make sure that the pilot line to the cuff is still intact. The capnograph adaptor or sampling line should be as close to the incisors as possible. When you minimize mechanical dead space you minimize the potential of rebreathing CO2.

Image from Grubb et al 2020
RVT measurint ET tube from the thoracic inlet to the incisors to help limit dead space and rebreathing of CO2.

Image taken by Jenny Gibbons
Correct placement of EtCO2 adapter on an anesthetized patient.
- If using a non-rebreathing anesthetic circuit, make sure to calculate an appropriate O2 flow rate (range 150-300ml/kg/min). Higher fresh gas flow rates are required to delivery fresh gas and eliminate waste anesthetic gas and CO2 and prevent rebreathing (GRUBB p42). If your O2 flow rate is too low the expired gas stays in the circuit, and the patient will rebreathe it. Increasing the flow rate can help clear the expired CO2 from the patient through the scavenge system.
- Check that the CO2 absorbent (Soda lime, Bara lime) is not exhausted. It is the presence of effective granules that insures that only exhaled O2, and anesthetic gas are rebreathed by the patient on the next inhalation. Exhausted granules will allow the CO2 to build up in the system allowing the patient to rebreathe CO2 and become hypercapnic. You can not rely on colour change alone!! The granules remove CO2 because the CO2 is an acid that is buffered by the CO2 absorbent, which is a base. This chemical reaction creates moisture, heat, and a change in pH. The colour indicators in the absorbent granules are pH sensitive so the pH change causes the colour (usually purple, blue or pink) to appear. Soda Lime often returns to there original colour after use, as the pH changes again. This does not mean your soda lime has restored capacity to absorb CO2-it is still exhausted. Dehydrated soda lime will not change colour as the chemical reaction can not occur without moisture. This can lead you to believe your soda lime is working when it is not! Fresh soda lime is easily crushed in between, gloved, fingers. Exhausted soda lime will be very hard and not easily crushed. Another way to check that your soda lime is working is to feel the canister that the CO2 absorbent granules are housed in. Active soda lime heats up as the chemical reaction is occurring. If you feel the canister during an anesthetic, it should be warm. If it is not warm, it is not working!! There are various guidelines for how often the CO2 absorbent should be changed. Depending on the type of granules used and the size of the canister the range is anywhere between 6-14 hours of anesthesia time. If you do not reach 6-14 hours of anesthesia time in a week, you may want to consider changing the CO2 absorbent anyways, as they will be slowly drying out. As stated previously, moisture is required for the chemical reaction in the soda lime to take place, ensuring the CO2 is absorbed. Consult the instruction manual for the CO2 absorbent granules your clinic uses to educate yourself on when they should be changed.
Exhausted CO2 absorbent (Soda Lime) granules.
Capnograph waveform when CO2 absorbent is exhausted. Note that the baseline is not returning to 0.
- Another reason you may see rebreathing of CO2 is if you have a faulty exhalation unidirectional (flutter) valve. When functioning properly, the unidirectional valves create a unidirectional flow of gases and prevent the rebreathing of exhaled gases prior to their exposure to CO2 absorbent. If these valves get stuck open for any reason, damage to valve, condensation within the dome of the valve, the patient will rebreathe CO2. It is recommended that the dome housing that covers the valves should be opened and the valves dried at the end of each anesthesia day to avoid them from sticking open. Tightly screw on the dome housing before next use. The valve should also be inspected and replaced if suspected wear and tear during routine maintenance to ensure their efficacy.
Capnograph waveform, EtCO2 and FiCO2 values on a patient whose anesthetic machine had a faulty exhalation unidirectional valve (stuck open).
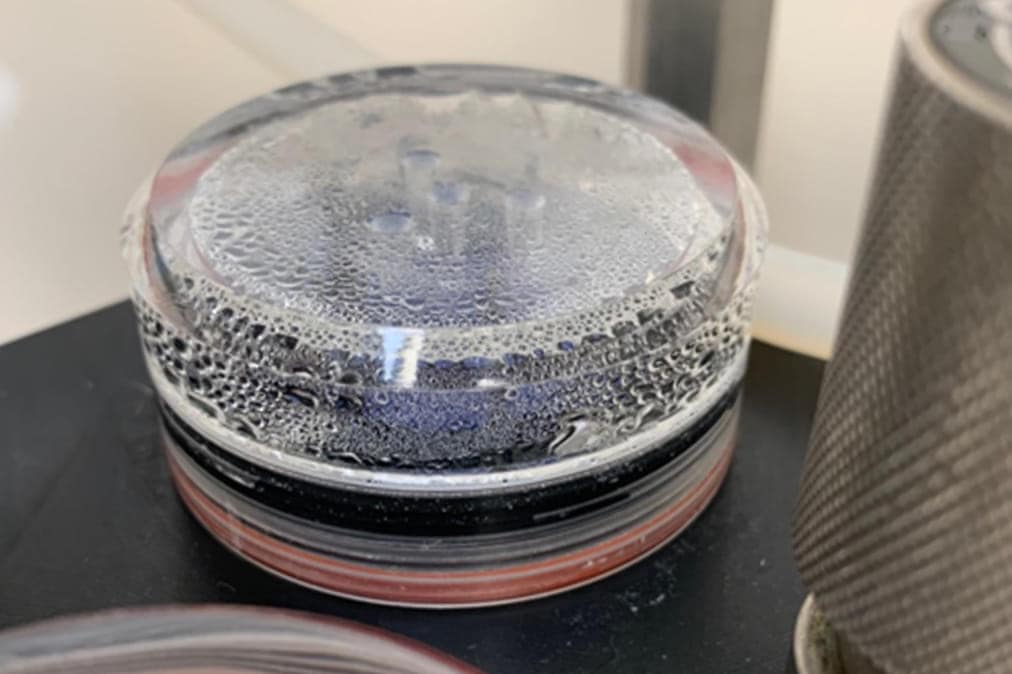
Condensation builds up in the dome of the exhalation valve, causing the exhalation valve to stay open.
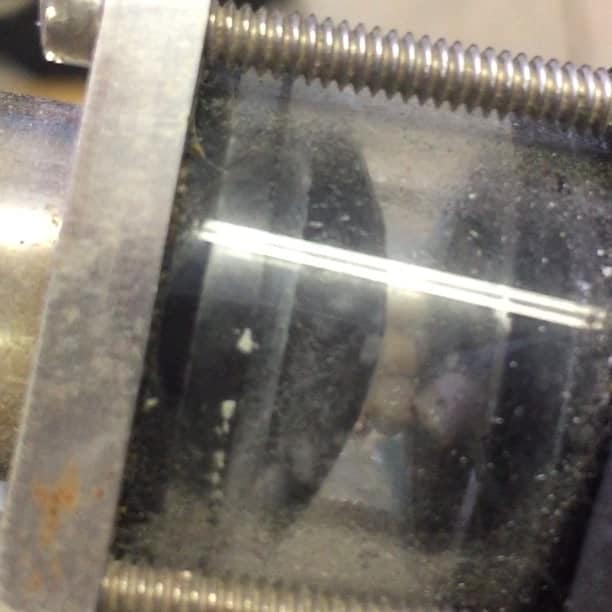
Image taken by Jenny Gibbons
Faulty exhalation unidirectional valve. Valve is stuck in the open position allowing rebreathing of CO2.
- Another thing you should check if your patient is rebreathing CO2 is your patient’s breathing circuit. If there are cracks or the inspiratory hose has pulled away from the end of the expiratory hose it will allow the mixture of fresh gas and exhaled gas and your patient will rebreathe CO2. A visual inspection of your circuit hoses before each use can verify the integrity of your circuit and prevent your patient from rebreathing CO2. You should check for leaks of the inner tube of a non-rebreathing system before each use. To do this (GRUBB):
- Set flow meter at 2L/min
- Occlude the inner tube with something small like the plunger to a syringe or your finger.
- If the inner tube is intact the flowmeter ball will drop in the flow tube because of the increase in back pressure.
- Immediately let off the pressure!

Image taken by Jenny Gibbons
Damage to the F circuit that caused the internal inspiratory hose has pulled away from the end of the external, expiratory hose allowing the patient to rebreathe CO2.
If the baseline on your capnograph waveform does not go back to zero and you have any value on your InCO2/FiCO2 other than zero, this can alert the registered veterinary technician that there is an issue with the anesthetic equipment. Whether it is increased mechanical dead space from a long ET tube, inadequate fresh gas flow on a non-rebreathing system, exhausted CO2 absorbent or faulty unidirectional valves or anesthetic circuits, catching these problems early is critical to the safety of the patient. Routine checks and maintenance of your anesthetic equipment can help catch these issues before the patient is even anesthetized. However, if you find yourself in a situation where your patient is rebreathing CO2 focus your troubleshooting efforts on your equipment to help to quickly solve the issue.
References
- Veterinary Anesthesia and Analgesia 6th edition, Lumb and Jones, 2024.
- Anesthesia and Pain Management for Veterinary Nurses and Technicians, Grubb et al, 2020.
- Anesthesia and Analgesia for Veterinary Technicians 5th edition, Thomas and Lerche, 2017.
- https://vetnurse.com.au/2015/09/14/changing-soda-lime/
- https://www.veterinarypracticenews.com/10-secrets-of-veterinary-anesthesia-machines/

Written by
Dr. Jenny Gibbons RVT, VTS (Anesthesia & Analgesia)
Graduated from the Veterinary Technology program at Ridgetown College and became a Registered Veterinary Technician that same year. Initially worked in research then made the transition to emergency medicine at the Veterinary Emergency Clinic. Always having an interest in anesthesia, when a position opened up in the surgery department at… [Read More]